Preoperative Evaluation of the Lung Cancer Resection Candidate
Peter J Mazzone
Posted: 03/09/2010; Expert Rev Resp Med. 2010;4(1):97-113. © 2010 Expert Reviews Ltd.
Abstract and Introduction
Abstract
Anatomical lung resection offers the best chance of cure for patients with localized lung cancer. Many people who have lung cancer have additional comorbidities, including other lung problems. Lung resection will affect our patient’s pulmonary function. When evaluating patients for lung resection we use measures of pulmonary function, predictions of postoperative lung function and measures of exercise capacity to determine their short- and long-term risks from resection. This article attempts to relate the evidence that is available regarding the physiologic evaluation of lung-resection candidates to guidelines that have been developed to help us coordinate our assessment. Testing algorithms are provided from these guidelines. In addition, perioperative considerations and alternative surgical approaches are discussed.
Introduction
Surgical resection has the greatest chance of curing patients with localized lung cancer. Unfortunately, only 20–30% of individuals with lung cancer are found to be candidates for lung resection, owing to the stage of their disease or associated comorbidities.[1,2] Many patients with lung cancer are elderly and have a history of cigarette use. Thus, those being evaluated for lung resection frequently have comorbidities. A report demonstrated that 37% of individuals who present with anatomically resectable disease are deemed not to be surgical candidates based on poor lung function alone.[3] Understanding the prognosis without surgery, the expected early morbidity from lung resection and the potential loss of lung function related to the resection helps us to understand the importance of the preoperative pulmonary evaluation of lung resection candidates.
Poor Prognosis Without Lung Resection
Many series have described very poor outcomes in those who are unable or unwilling to have a curative intent lung resection for early-stage lung cancer. Without surgical treatment:
- Patients who had been screen-detected stage I had a median survival of 25 months without surgical treatment. Symptom-detected stage I patients had a median survival of 13 months in one report;[4]
- Screen-detected stage I patients had 5- and 10-year survival rates of 16.6 and 7.4%, respectively;[5]
- Individuals with squamous cell carcinoma on sputum cytology with negative chest imaging had 5- and 10-year lung cancer survival rates of 53.2 and 33.5%, respectively;[6]
- A total of 57 patients with resectable cancer had a median survival of 15.6 months, compared with 30.9 months in 346 patients who completed resection.[7]
Surgical Morbidity & Mortality
In the past decade, several large series have described modern operative mortality and early complications of lung resection. Others have attempted to identify factors that are associated with immediate postoperative complications:
- A survey conducted in 2001 from 729 hospitals in the USA[2] reported on 11,668 surgically treated patients. The cohort was representative of the group that develops lung cancer. A total of 47% were aged 70 years or more and 76% had comorbidities. Perioperative mortality was 5.2%;
- A report from 63 large institutions described 1023 lung cancer patients undergoing resection as part of a randomized trial (lymph node sampling vs lymph node dissection).[8] The median age of the group was 68 years. The operative mortality in this group was 1.3%, with complications reported in 38% of the patients;
- A report of 46,951 lung cancer resections, with data obtained from the Nationwide Inpatient Sample data set from 1998 to 2004, reported an in-hospital mortality of 3.5%. The mean age of the patients was 66.3 years;[9]
- A report of 512,758 lung resections performed from 1988 to 2002, with data obtained from the national Hospital Discharge Survey, reported an in-hospital mortality of 4.8% over that time. Over time, there were increases in the average age (63.2 years), the proportion of women (49.6%) and the proportion of lobectomies. There was a decrease in the hospital length of stay (9.1 days) and in listed complications (21.8%);[10]
- A total of 9033 pulmonary resections for primary lung cancer were analyzed using information recorded in the Society of Thoracic Surgeons General Thoracic Surgeons database from 1999 to 2006. There were equal portions of men and women, with a median age of 67 years. Comorbidities were present in 79% of the group. Median length of stay was 5 days, operative mortality was 2.5% and postoperative complications occurred in 32% of the patients;[11]
- A total of 4979 patients from the Society of Thoracic Surgeons General Thoracic Surgery database were reviewed to develop a risk-adjustment model for outcomes after lobectomy. Prolonged length of stay (>14 days) was found to be a surrogate of postoperative events and, thus, was used to develop the model. Predictors of a prolonged length of stay included age, Zubrod score, being male, the American Society of Anesthesiology score, insulin-dependent diabetes mellitus, renal dysfunction, induction therapy, percentage predicted forced expiratory volume in 1 s (FEV1) and smoking;[12]
- A prospective evaluation of 168 patients undergoing lung resection demonstrated that up to 25% develop postoperative pneumonia. This increases to 48% if the airways are colonized at the time of surgery. Other predictors included the presence of chronic obstructive pulmonary disease (COPD), being male and the extent of resection. Standard measures of outcome, including mortality, are increased if pneumonia develops;[13]
- Active smoking, dyspnea, age, the extent of surgery, vascular disease, diabetes mellitus and dysrhythmias have been variably associated with an increased risk of complications and/or mortality.[1,14–16]
Impact on Pulmonary Function of Standard Resection
It is important to consider the impact of resection on lung function and quality of life after operative recovery. Reports of the expected loss of lung function and exercise capacity are available. Variables that have been considered in some of the reports include the time postresection that loss of function is being assessed, the extent of the resection (lobe vs pneumonectomy), the presence of COPD at baseline (or the impact of the preoperative lung function) and the area of the lung being removed. The following points illustrate the available literature:
- Unselected series have recorded postoperative FEV1 values of 81–91% of preoperative values when measured up to 6 months after lobectomy, and 64–66% after pneumonectomy;[17–20]
- Unselected series have recorded postoperative diffusing capacity for carbon monoxide (DLCO) values of 82–89% of preoperative values when measured up to 6 months after lobectomy and 80% after pneumonectomy;[19,20]
- Unselected series have recorded maximal oxygen consumption (VO2 max) values of 87–100% of preoperative values when measured up to 6 months after lobectomy, and 72–89% after pneumonectomy.[17–20] One study assessed VO2 max in pneumonectomy patients 3 years after resection. Values were 70% of baseline;[21]
- Series that included only COPD patients, or compared patients with COPD with those without, described a smaller decline in FEV1 in those with COPD who had a lobectomy (0–8%) compared with those without COPD (16–20%).[22,23,20] The fall in DLCO and VO2 max was more variable (3–20% for DLCO; 0–21% for VO2 max);[23,20]
- Measures of pulmonary function and exercise capacity increased from the time of surgery through at least 6 months in those who underwent lobectomy. Significant improvements were not seen beyond 3 months postpneumonectomy;[17,18,20]
- The location of the resection can influence the degree of loss of lung function;[20]
- The quality of life of individuals with resectable lung cancer tends to be lower than the general population. Physical measures have been shown to decline at the 1-month postoperative time but return to baseline by 3 months postoperatively. Mental measures may not decline throughout. Quality-of-life measures have a poor correlation with measures of pulmonary function or other high-risk patient features.[24]
The aforementioned studies demonstrate a poor prognosis for lung cancer when surgery is not an option, a reasonable morbidity and mortality related to standard resection despite an ill population, and a modest decline in lung function and exercise capacity from resection. In the remainder of this article, the author reviews the evidence that supports various means of assessing an individual’s pulmonary fitness, considerations related to preparing them for resection and opportunities for resection when standard criteria are not met. The evidence in each area is related to two recent guidelines published by the American College of Chest Physicians (ACCP)[25] and the European Respiratory Society (ERS) with the European Society of Thoracic Surgery (ESTS).[26]
Age
Evidence
Age is an identified as an independent predictor of complications from lung resection. Elderly age influences decisions related to resection.[27] A large study reported surgical rates of 14% in those aged over 70 years and 26% in those under 70 years of age. Pneumonectomy rates were 27% in those aged over 70 years and 37% in those under 70 years of age.[1]
There are many series describing outcomes of lung resection in the elderly.[28–41] These series span a long period of time, including different populations of patients. Outcomes reported and the period of follow-up have varied. The general concerns raised by the literature include a higher operative mortality in the elderly, relatively high operative risks for pneumonectomy and an increased risk of postoperative complications. The presence of comorbidities are more predictive of outcome than age alone.[40–41] Those who are elderly and are able to tolerate resection, survive longer than those who cannot undergo surgery (Table 1).
Table 1. Lung resection in the elderly.
| Author (year) |
Age (years) |
Operative mortality (%) |
Survival (%), years |
Ref. |
| Evans (1973) |
65–74
>75 |
19
26.7 |
48, 4 L
31, 4 P |
[156] |
| Kirsh et al. (1976) |
>70 |
14 |
30, 5 O
0, 5 P |
[28] |
| Breyer et al. (1981) |
>70 |
3 |
42, 5 L
13, 5 P |
[29] |
| Nagasaki et al. (1982) |
>70 |
 |
 |
[30] |
| Ginsberg et al. (1983) |
60–79
>80 |
7
8.1 |
 |
[31] |
| Sherman et al. (1987) |
>70 |
9.4 |
36, 5 |
[32] |
| Ishida et al. (1990) |
>70 |
3 |
48, 5 |
[33] |
| Shirakusa et al. (1989) |
>80 |
12 |
55, 5 |
[34] |
| Roxburgh et al. (1991) |
>70 |
4.7 – L
9.1 – P |
73, 2
67, 4 |
[35] |
| Riquet et al. (1994) |
>75 |
12.1 |
16, 5 |
[36] |
| Massard et al. (1996) |
>70 |
6.6 –L
10 – P |
33, 5 |
[37] |
| Pagni et al. (1997) |
>80 |
3.7 |
86, 1
43, 5 |
[38] |
| Port et al. (2004) |
>80 |
1.6 |
38, 5
82, 5 IA |
[39] |
| Birim et al. (2003) |
>70 |
3.2 |
37, 5 |
[41] |
| Brock et al. (2004) |
>80 |
8.8 |
73, 1
34, 5 |
[40] |
IA: Stage IA; L: Lobectomy; O: Overall; P: Pneumonectomy.
Guidelines
The ACCP guidelines recommended that patients with lung cancer are not denied lung resection surgery on the grounds of age alone.
Standard Lung Function Testing
Many measures of pulmonary function have been studied as predictors of risk for lung resection. The following section describes the guidelines and evidence surrounding the use of the two most commonly applied tests, FEV1 and DLCO.
Evidence
FEV1 is able to help predict the risk for postoperative complications including death. Absolute values and percent predicted values have been used.[42] It has been difficult to identify an absolute cut-off value, capable of consistently predicting surgical and long-term risks. An older series reported that 40% of patients with an FEV1 under 2.0 l and age over 60 years did poorly.[43] Preoperative values of 2 l for pneumonectomy and 1.5 l for lobectomy have been suggested as cut offs to allow surgery to occur without the need for additional testing. Other series have confirmed that individuals whose FEV1 is above these thresholds have a low risk of mortality.[43–45] Absolute FEV1 values represent a range of lung function based on an individual’s age, sex and height. Thus, FEV1 values expressed as percentages of normal have been used. In one report, those with a preoperative FEV1 under 60% predicted had an odds ratio of 2.7 for respirator complications and 1.9 for 30-day mortality.[42] Another group reported a mean FEV1 of 75% predicted in uncomplicated resections and 66% in complicated resections.[7] A value of 80% predicted or higher has been suggested in a reported algorithm as a cut off, which if met would permit resection without the need for additional testing.[46]
DLCO is a predictor of postoperative complications including death, length of hospital stay and hospital costs.[47–49] As mentioned previously, absolute cut offs are not clearly established in the literature. Individuals with a preoperative DLCO less than 60% predicted had a higher risk of respiratory complications, a higher risk of hospitalizations for respiratory compromise and lower median dyspnea scores in one report.[50] In another report, the mean DLCO was 77% predicted in those without complications and 67% in those with.[7] The FEV1 and DLCO have only a modest correlation with each other. A report found that 43% of patients with a FEV1 over 80% predicted had a DLCO under 80% predicted.[51]
Guidelines
The ACCP guidelines state that in patients being considered for lung cancer resection, spirometry is recommended. If the FEV1 is over 80% predicted or over 2 l and there is no evidence of either undue dyspnea on exertion or interstitial lung disease, the patient is suitable for resection including pneumonectomy without further physiologic evaluation. If the FEV1 is over 1.5 l and there is no evidence of either undue dyspnea on exertion or interstitial lung disease, the patient is suitable for a lobectomy without further physiologic evaluation.
The ACCP guidelines also state that in patients being considered for lung cancer resection, if there is evidence of either undue dyspnea on exertion or interstitial lung disease, even though the FEV1 might be adequate, measuring DLCO is recommended.
The ERS/ESTS guidelines state that DLCO should be routinely measured during preoperative evaluation of lung resection candidates, regardless of whether the spirometric evaluation is abnormal.
Predicted Postoperative Lung Function
Evidence
Three strategies have been used to predict pulmonary function after lung-resection surgery.
Segment Methods When using a segment method, postoperative pulmonary function is predicted by calculating the portion of all bronchopulmonary segments that will remain after resection, then multiplying this portion by the preoperative lung function value. In a study that used 19 total segments as the starting value (ten on the right and nine on the left), the predicted postoperative lung function was found to have a good correlation with actual lung function for those undergoing lobectomy (r = 0.867), and a fair correlation (r = 0.677) for those undergoing pneumonectomy.[52] The actual lung function was consistently underestimated (by 250 ml for lobectomy and 500 ml for pneumonectomy). A second segment method based calculations on the total number of subsegments (42) then corrected for those that were obstructed by tumor preoperatively.[53] When a regression equation relating the predicted and measured lung function was applied, a good correlation between predicted and actual lung function was found (r = 0.821).
Radionuclide Scanning Techniques When using radionuclide scanning techniques, the relative function of the portion of lung to be resected is estimated by quantifying either the perfusion or ventilation to that area. Postoperative lung function is then calculated as the product of the preoperative function and the portion of lung function that will remain after resection as estimated by the scan. Studies using radionuclide scanning techniques have shown a fair-to-good correlation of the predicted and actual postoperative FEV1 (r = 0.63–0.88).[54–57] The correlation of predicted postoperative and actual DLCO has been as low as 0.68.[57]
Some studies have suggested the predictive capabilities of radionuclide scanning are less than ideal. One study found that only 41 out of 159 predicted postoperative values were within 5% of actual values.[58] Another found values of imprecision of 18–21%, despite showing reasonable correlation.[59] The estimates of postoperative lung function were better for lobectomy in the right lung than in the left. As with the segment methods, FEV1 was consistently underestimated, particularly if the starting value was lower.
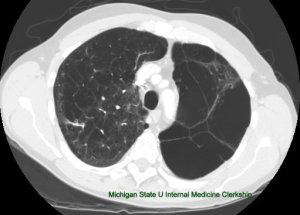
Quantitative Computed Tomography When using quantitative computed tomography (CT) scanning, the volume of lung with attenuation between -500 and -910 Hounsfield units makes up the estimated functional lung volume. The functional lung volume in the area to be resected is calculated as a portion of the total functional lung volume. Using this technique, predicted postoperative lung function has correlated as well as or better than that calculated by radionuclide quantitative perfusion imaging in some studies.[60,61] As with the other techniques, predictions of postoperative lung function often underestimate actual lung function in those with COPD.[62] One study used quantitative CT scanning to develop a regression equation to estimate the predicted postoperative oxygen saturation, which has correlated with postoperative recovery time and cardiopulmonary complications.[63]
Comparison A study of 44 subjects compared predictions of postoperative lung function (FEV1, forced vital capacity [FVC], DLCO and VO2 max) based on five methods (radionuclide perfusion scan, quantitative CT and three segment methods – a standard segment method, functional segment method and subsegment method) with actual values obtained at 6 months post-resection. Perfusion imaging outperformed other methods for all measures regardless of the extent of resection or degree of obstruction. All other methods performed well in those who had a lobectomy. Segment methods did not perform well in those who had a pneumonectomy.[19] This finding was confirmed in a study of 32 patients who underwent pneumonectomy. Perfusion imaging prediction outperformed the segment method at the 3-year postresection time point.[21]
Guidelines
The ACCP guidelines state that in patients being considered for lung cancer resection, if either the FEV1 or DLCO are under 80% predicted, it is recommended that postoperative lung function be predicted through additional testing.
The ERS/ESTS guidelines state that the predictive postoperative (ppo)FEV1 should not be used alone to select patients with lung cancer for lung resection, particularly patients with moderate-to-severe COPD. It tends to underestimate the functional loss in the early postoperative phase and does not appear to be a reliable predictor of complications in COPD patients.
The ERS/ESTS guidelines also state that the first estimate of residual lung function should be calculated based on segment counting. Only segments not totally obstructed should be taken into account: the patency of bronchus (bronchoscopy) and segment structure (CT scan) should be preserved.
Furthermore the ERS/ESTS guidelines state that patients with borderline function should need imaging-based calculation of residual lung function: ventilation or perfusion scintigraphy before pneumonectomy, or quantitative CT scan before lobectomy or pneumonectomy.
Evidence
The ppoFEV1 is an independent predictor of complications, including mortality in some reported series.[64–66] Absolute values for ppoFEV1 that would permit resection have been difficult to find. Examples from the literature include:
- The mean ppoFEV1 in individuals who developed respiratory failure after surgery was 37.6% predicted normal and 42.3% in those who died. All individuals with a ppoFEV1 of less than 30% predicted normal developed respiratory failure or died;[67]
- A total of 70% of individuals with a ppoFEV1 less than 35% predicted normal experience complications;[68]
- Individuals with a ppoFEV1 greater than 34% predicted or greater than 58% of the preoperative value have a decreased postoperative mortality;[69,70]
- A ppoFEV1 greater than 40% predicted normal was found to identify those at risk for mortality, with no deaths in those greater than 40%, and a 50% mortality rate in those less than 40%.[47]
The ppoFEV1 has been used to permit individuals to have resection who may have been denied on the basis of their absolute FEV1 value alone. Examples from the literature include:
- Individuals with an FEV1 less than 2 l to undergo pneumonectomy if their ppoFEV1 was over 800 cc.[71] The operative mortality in these patients was 15%;
- A study using the same criteria reported 61% survival at 1 year, 34% at 2 years and 5% at 5 years;[72]
- Another group allowed resection if the ppoFEV1 was greater than 1 l. An operative mortality of 6.7% was found in those who had pneumonectomy. A total of 22 individuals who had preoperative FEV1 values less than 2 l, and 40 with FEV1 values less than 1.5 l would have been denied pneumonectomy and lobectomy, respectively, if not for the ppoFEV1 value. There were no postoperative deaths in these individuals;[44]
One study found the ppoDLCO to be a predictor of mortality, while others determined it to be an independent predictor of pulmonary complications, morbidity and death.[66,73–75] A ppoDLCO under 40% was reported to be a predictor of postoperative complications in patients with a normal FEV1.[51] A combined value, termed the predicted postoperative product (PPP), has been studied as a risk predictor. The PPP is the product of the ppoFEV1 and ppoDLCO. It was found to be the best predictor of surgical mortality in one study.[76] A PPP less than 1650 was found in 75% of those who died and 11% of those who survived surgery.
Guidelines
The ACCP guidlelines state that in patients with lung cancer who are being considered for surgery, either a product of % ppoFEV1 and % ppoDLCO of under 1650% ppo or an FEV1 of under 30% ppo indicates an increased risk for perioperative death and cardiopulmonary complications with standard lung resection. It is recommended that these patients should be counseled about nonstandard surgery and nonoperative treatment options for their lung cancer.
The ERS/ESTS guidelines state that a ppoFEV1 value of 30% predicted is suggested to be a high-risk threshold for this parameter when included in an algorithm for assessment of pulmonary reserve before surgery. The ERS/ESTS guidelines also state that a ppoDLCO value of 30% predicted is suggested to be a high-risk threshold for this parameter when included in an algorithm for assessment of pulmonary reserve before surgery.
Exercise Testing
Exercise testing has been used to assess a patient’s fitness for lung resection. Symptom-limited cycle ergometry, exercise oximetry, stair climbing and shuttle walking have all been reported to be able to predict complications.
Evidence
Exercise capacity, measured as the VO2 max during symptom limited cycle ergometry, has been reported to be a predictor of postoperative complications, including postoperative and long-term mortality.[7,77–85] A sample of the available literature is outlined in Table 2. A meta-analysis of available trials demonstrated that patients without complications had significantly higher levels of VO2 max and percentage predicted (by a mean of 3 ml/kg/min and 8%, respectively).[86]
Table 2. Cardiopulmonary exercise testing in the assessment of the lung resection candidate.
| Author (year) |
Findings VO2 max (ml/kg/min unless stated) |
Ref. |
| Olsen et al. (1989) |
Mean VO2 max 11.3 in those without complications and 7.8 in those with |
[80] |
| Bolliger et al. (1995) |
ppoVO2 max < 10 associated with 100% mortality; mean VO2 max 62.8% predicted in those with complications, 84.6% in those without; ppoVO2 max 44% predicted in those with complications, 68% in those without |
[81] |
| Bolliger et al. (1995) |
Mean VO2 max 84% predicted in those without complications and 61% in those with VO2 max < 60% predicted in nine patients – eight had complications, three died |
[82] |
| Larsen et al. (1997) |
High mortality rate if VO2 max < 50% predicted |
[83] |
| Brutsche et al. (2000) |
VO2 max and extent of resection were independent predictors of complications |
[84] |
| Smith et al. (1984) |
All with VO2 max < 15 had complications |
[157] |
| Bechard et al. (1987) |
29% mortality with VO2 max < 10, no morbidity or mortality if >20 |
[158] |
| Loewen et al. (2007) |
VO2 max of 65% predicted a predictor of complications and poor outcome |
[7] |
| Win et al. (2005) |
VO2 max 91.7% predicted in those with a satisfactory outcome, 65.9% in those with a poor outcome |
[85] |
| Brunelli et al. (2009) |
No deaths if VO2 max >20, 13% mortality if VO2 max was < 12 |
[87] |
ppo: Predictive postoperative; VO2 max: Maximal oxygen consumption.
Exercise capacity has been used to determine if individuals with unacceptable lung function by other measures might be able to tolerate resection. One study permitted otherwise inoperable patients to undergo resection if their VO2 max was greater than 15 ml/kg/min.[77] Of the eight individuals who qualified, there were two complications and no deaths. Another study permitting resection when the VO2 max was greater than 15 ml/kg/min found a 40% incidence of complications but no deaths in the 20 patients who qualified.[78] A total of five individuals had surgery but did not reach 15 ml/kg/min. Of these five, one death was observed. The median survival in those who qualified for surgery based on the exercise test result was 48 months, while the survival in 37 individuals who did not meet criteria was 17 months. Another study concluded the risks were acceptable with a VO2 max of 10 ml/kg/min or greater, three flights of stairs climbed for a lobectomy and five flights for a pneumonectomy.[79] A report of 204 patients who had cardiopulmonary exercise testing (CPEX) regardless of their standard lung function parameters and went on to a lobectomy or pneumonectomy was published. They found that CPEX did not add to risk stratification if the FEV1 and DLCO were over 80%. In the group with either FEV1 or DLCO under 80%, but both ppoFEV1 and ppoDLCO over 40%, there were five deaths, three of which occurred in patients with a peak VO2 under 12 ml/kg/min. Three patients in this group were found to have cardiac ischemia requiring intervention at the time of their CPEX. They found that patients with ppoFEV1, ppoDLCO or both under 40% predicted could tolerate major resection if their peak VO2 max was over 10 ml/kg/min. Even those with a ppoFEV1 under 30% or PPP under 1650 tolerated resection reasonably well if the VO2 peak was over 10 ml/kg/min.[87]
Results from CPEX testing other than VO2 max have also been assessed as predictors of outcome. Oxygen delivery was found to discriminate between fatal and nonfatal complications. Those with fatal complications had an oxygen delivery less than 500 ml/min/m2, while those with nonfatal complications or no complications had an oxygen delivery greater than 560 ml/min/m2.[88] The change in diffusing capacity with exercise has also been studied.[89] An increase of less than 10% of the predicted DLCO occurred in all who had complications, while only 10% of those with an increase greater than 10% developed a complication. An increase of less than 5% of predicted DLCO was associated with mortality.
Guidelines
The ACCP guidelines state that in patients with lung cancer who are being considered for surgery, either an FEV1 of under 40% ppo or a DLCO of under 40% ppo indicates an increased risk for perioperative death and cardiopulmonary complications with standard lung resection. It is recommended that these patients undergo exercise testing preoperatively.
The ERS/ESTS guidelines state that exercise tests should be indicated in all patients undergoing surgery for lung cancer with FEV1 or DLCO under 80% of normal values. The ERS/ESTS guidelines also state that cardiopulmonary exercise testing is performed in a controlled environment, and is reproducible and safe. VO2 peak measured during an incremental exercise on treadmill or cycle should be regarded as the most important parameter to consider, as a measure of exercise capacity and as highly predictive of postoperative complications.
The ACCP guidelines state that in patients with lung cancer being considered for surgery, a VO2 max of under 10 ml/kg/min indicates an increased risk for perioperative death and cardiopulmonary complications with standard lung resection. These patients should be counseled about nonstandard surgery and nonoperative treatment options for their lung cancer. The ACCP guidlines also state that patients with lung cancer being considered for surgery who have a VO2 max of under 15 ml/kg/min and both an FEV1 and a DLCO of under 40% ppo are at an increased risk for perioperative death and cardiopulmonary complications with standard lung resection. It is recommended that these patients be counseled about nonstandard surgery and nonoperative treatment options for their lung cancer.
The ERS/ESTS guidelines state that the following basic cut-off values for VO2 peak should be considered: over 75% predicted or over 20 ml/kg/min qualifies for pneumonectomy; under 35% predicted or under 10 ml/kg/min indicates high risk for any resection. Evidence is not sufficient to recommend cut-off values for lobectomy.
Evidence
Exercise Oximetry The predictive value of oxygen desaturation has varied in the literature. A 4% or greater desaturation during standardized exercise has performed better than measures of FEV1 and DLCO in predicting respiratory failure, major morbidity, intensive care unit admission, length of stay and home oxygen requirements in some studies.[90,91] Another study that looked at oxygen desaturation during a shuttle walk test did not find it to be predictive of outcome.[92]
Stair Climbing The number of steps climbed has shown a fair correlation with FEV1, DLCO, VO2 max and minute ventilation.[93,94] The ability to climb stairs has been used to estimate the risk of complications and mortality related to lung resection. A sample of the literature includes:
- The ability to climb three flights of stairs (25 steps per flight) was associated with lower rates of postoperative intubation, fewer complications and a shorter hospital stay;[95]
- A study of high-risk individuals showed a climb of 44 stairs (each 0.17 m high) could predict a good outcome;[96]
- A study of 160 lung resection candidates found the altitude reached during the stair climb was the only independent predictor of complications (14.6 m in those with complications versus 20.6 m in those without complications). The authors suggested a cut off of 12 m be used to predict the tolerability of resection;[97]
- A report of 640 patients who performed stair climbing prior to resection showed that the altitude reached was associated with cardiopulmonary complications, mortality and costs. A cut off of 12 m altitude had a positive predictive value of 40% for morbidity and 13% for mortality with a negative predictive value of 78% for morbidity and 97% for mortality;[98]
- Those who are unable to perform a maximal stair climbing test due to underlying comorbidities have been found to have an increased risk of mortality after major lung resection.[99]
Other Measures of Exercise Capacity The distance obtained during a shuttle walk test, where an individual walks back and forth over a defined distance at an incremental and progressive rate, has correlated well with VO2 max obtained on a treadmill. Walking 25 shuttles (10 m each) approximated a VO2 max of 10 ml/kg/min.[100,101] Some have suggested that the shuttle walk distance may not predict surgical outcome.[102]
A 6-min walk test distance of 1000 feet or greater has been found to predict positive outcome.[96] It was the best predictor of postoperative respiratory failure in another.[76]
Guidelines
The ACCP guidelines state that patients with lung cancer being considered for surgery who walk under 25 shuttles on two shuttle walks or less than one flight of stairs are at increased risk for perioperative death and cardiopulmonary complications with standard lung resection. These patients should be counseled about nonstandard surgery and nonoperative treatment options for their lung cancer.
The ERS/ESTS guidelines state that shuttle walk test distance underestimates exercise capacity at the lower range and was not found to discriminate between patients with and without complications. Thus, it should not be used alone to select patients for operation. It could be used as a screening test: patients walking less than 400 m may have VO2 peak under 15 ml/kg/min. The ERS/ESTS guidelines also state that the standardized symptom-limited stair climbing test is a cost-effective test capable of predicting morbidity and mortality after lung resection better than traditional spirometry values. It should be used as a first-line functional screening test to select those patients that can undergo safely to operation (height of ascent >22 m) or those who need more sophisticated exercise tests in order to optimize their perioperative management.The ERS/ESTS guidelines then state that the 6-min walk test should not be used to select patients for operation.
Algorithms
Based on the above listed guidelines, both the ACCP and ERS/ESTS have produced algorithms for the preoperative pulmonary evaluation of lung cancer resection candidates (Figures 1 & 2).[25,26] The major differences in the algorithms are the recommendations for when to obtain a DLCO measure, and when to perform exercise testing. Minor differences in cut-off values for the various measures exist. The evidence used to support the content of these algorithms has been described in detail previously. Clearly, this evidence has been interpreted differently by the two groups. It is important to note that the two evaluation algorithms have not been validated, compared with each other, or compared with other existing algorithms.[45,46,102,103]

Figure 1. Preresection testing algorithm proposed by the American College of Chest Physicians.
CPET: Cardiopulmonary exercise testing; CT: Computed tomography; CXR: Chet x-ray; DLCO: Diffusing capacity for carbon monoxide; FEV1: Forced expiratory volume in 1 s; ppo: Predictive postoperative; VO2 max: Maximal oxygen consumption.
Reproduced with permission from [25].
Figure 2. Preresection testing algorithm proposed by the European Respiratory Society-European Society of Thoracic Surgeons.
DLCO: Diffusing capacity for carbon monoxide; FEV1: Forced expiratory volume in 1 s; ppo: Predictive postoperative.
Reproduced with permission from [26].
Alternative Surgeries
Evidence
Lung Volume Reduction Surgery In select patients with severe emphysema, removal of the most emphysematous portion of their lung can lead to improvements in lung function.[104–106] Individuals with severe emphysema are at risk for lung cancer due to shared risk factors. Lung nodules are often found during the preoperative evaluation. Localized lung cancer has been found in approximately 5% of those undergoing lung volume reduction surgery.[107] Resection has been reported to be possible in individuals who do not meet standard criteria by using lung volume reduction surgery where appropriate. A lobectomy may be performed if a cancer is present in the lobe that will undergo lung volume reduction, whereas lesser resections are combined with volume reduction if cancer is found in a different lobe. A summary of some of the case series described is given in Table 3.[22,108–113] In addition to improvements in lung function, properly selected candidates have seen durable quality-of-life improvements, similar to those without lung cancer.[113]
Table 3. Outcomes of nodule resections during lung volume reduction surgery.
| Author (year) |
Patients (n) |
Cancer (n) |
Preop FEV1 (% predicted) |
Postop FEV1 (% predicted) |
Mortality (%) |
Ref. |
| Choong et al. (2004) |
21 |
21 |
29.0 |
40.0 |
0 |
[108] |
| Edwards et al. (2001) |
14 |
14 |
40.7 |
41.5 |
14 |
[22] |
| DeRose et al. (1998) |
14 |
9 |
27.0 |
35.0 |
7 |
[109] |
| DeMeester et al. (1998) |
5 |
5 |
29.6 |
42.3 |
0 |
[110] |
| Ojo et al. (1997) |
11 |
3 |
26.2 |
38.5 |
0 |
[111] |
| McKenna et al. (1996) |
51 |
11 |
21.7 |
49.0 |
0 |
[112] |
| Pompeo et al. (2003) |
16 |
16 |
0.92* |
1.20* |
0 |
[113] |
*Actual value in liters as % predicted not available.
FEV1: Forced expiratory volume in 1 s; Postop: Postoperation; Preop: Preoperation.
Sublobar Resections For early-stage lung cancer, the resection of choice is a lobectomy. In general, those who undergo a lobectomy have a lower rate of locoregional recurrence than those who have a sublobar resection.[114] There is evidence that sublobar resections still play a role in lung cancer treatment, particularly in those at most risk from a standard resection. The FEV1 is a significant prognostic factor for death by nonlung cancer causes in individuals with stage I lung cancers.[115] Thus, individuals with a very low FEV1 may not survive long enough to enjoy the benefits of lobectomy for reasons unrelated to their lung cancer. The literature in this area is difficult to interpret, as many studies have reported contradictory findings. In general, the age of the patient and the size of the tumor have been reported to influence the potential risks and benefits of sublobar resections. Acceptable morbidity and mortality has been reported in series of patients with what would be considered prohibitively low pulmonary function measures by most guidelines. A sample of the literature follows:
- A report of 14,555 patients from the Surveillance, Epidemiology and End Results (SEER)’s registry who had lung resection for stage I or II lung cancer found a benefit from lobectomy over a sublobar resection in younger individuals. The difference in survival disappeared after 71 years of age;[116]
- One report found 5-year survivals of 92.4, 96.7 and 85.7% for lobectomy, segmentectomy and wedge resection, respectively, in tumors that were 20 mm in diameter or smaller.[117] For tumors larger than 20 mm, the survival gaps were wider at 87.4, 84.6 and 35.4% for lobectomy, segmentectomy and wedge resection, respectively. None with a tumor larger than 30 mm who had a wedge resection survived at 5 years;
- No difference in oncologic outcome between anatomical segmentectomy and lobectomy was noted for tumors less than 2 cm in diameter;[118]
- In 784 individuals resected for stage I lung cancer, including 207 who had sublobar resections, the hazard ratio for disease-free survival and overall survival in those who had a sublobar resection was 1.2 and 1.39, respectively.[119] When divided into stage IA and IB, the entire difference appeared to come from the stage IB group;
- A report of 215 patients with T1N0M0 lung cancer, 147 treated with lobectomy, 47 with wedge resection and 19 with radiation therapy, found 1- and 5-year survival rates of 97 and 68% for lobectomy, 98 and 74% for wedge resection, and 80 and 39% for radiation therapy, respectively;[120]
- Another group reported resection outcomes of 219 patients with stage IA lung cancer, with 117 treated with lobectomy, 60 with video-assisted thoracoscopic surgery (VATS) wedge resection, and 42 with open wedge resection.[121] The corresponding 1- and 5-year survivals were 91 and 70%, 95 and 65%, and 94 and 58%, respectively. The noncancer death rate was 38% in the wedge groups combined and 18% in the lobectomy group;
- In some populations (e.g., adenocarcinoma in a Japanese study), limited resection has been reported to uniformly lead to cure;[122]
- Some have shown that anatomical segmentectomies lead to similar outcomes when compared with lobectomies with less loss of lung function and better oncologic results when compared with wedge resections.[123] Others have suggested wedge resection leads to similar oncologic results when compared with lobectomy for stage I lesions.[124] Still, others have reported lobectomy to be superior to wedge resection mainly for smaller tumors;[125]
- Sublobar resections have been reported to be safely performed in individuals with poor lung function. A report of 100 individuals with a preoperative FEV1 less than 35% predicted showed a 30-day postoperative mortality of 1% and a complication rate of 36%.[126] A total of 65% of resections were thoracoscopic wedge resections, and 8% included a lung volume reduction procedure;
- Individuals with poor lung function who underwent resection were more likely to survive the perioperative period if they had a performance status of less than 2, less than two concomitant diseases and COPD as the cause of their low FEV1.[127]
Changes in Pulmonary Function with Sublobar Resection There is not much literature regarding the differences in loss of pulmonary function when a lobectomy is performed compared with when a sublobar resection is performed. One study reported the 12-month postoperative FEV1 to be 93.3% of the preoperative value in patients with normal lung function who underwent segmentectomy.[128] This was compared with a value of 87.3% of the preoperative value in those who had a lobectomy. Another report comparing changes in pulmonary function after lobectomy and segmentectomy for stage I lung cancer found that the FVC, FEV1, maximum voluntary ventilation and DLCO all decreased after lobectomy.[129] Only the DLCO was decreased in those who had a segmentectomy. A final report reviewed 40 patients who had undergone thoracotomy – 13 had a wedge resection, 14 a lobectomy and 13 a thoracotomy alone due to finding an inoperable tumor.[130] There was no decline in measures of pulmonary function or exercise capacity in the wedge resection group. Similar declines were seen in the lobectomy and thoracotomy alone groups (perhaps a result of progression of the tumor or the effect of radiation therapy in the thoracotomy alone group).
Difficulties with Sublobar Resections Accurate staging, obtaining clean resection margins, and conversion to larger surgeries are potential problems with sublobar resections. A sample of the literature follows:
- One study investigated the feasibility of performing thoracoscopic wedge resections with radiation therapy for clinical T1 lesions in individuals with compromised cardiopulmonary status.[131] Clinical staging was often inaccurate, with 28% of patient upgraded and 17% found to have benign lesions at resection. Conversion to thoracotomy was required in 13% of T1 cancers and 31% of T2 cancers. Resection margins were positive in 6% of T1 cancers and 23% of T2 cancers. Operative failure rates were 22% for T1 cancers and 50% for T2 cancers. Pathologically staged T1 lesions were successfully resected in 75% of cases with narrow resection margins noted;
- Another study reviewed the pathology of 31 T1N0M0 lesions that had been diagnosed by wedge resection, which then proceeded to completion lobectomy.[132] They found the average microscopic margin was 2.3 mm and noted microscopic growth beyond the gross perimeter of 7.4 mm. A total of 17 of the lobectomy specimens were free of cancer while cancer was found in the other 14;
- One group reported 167 stage IB patients, 126 of whom received a lobectomy and 41 a sublobar resection with intraoperative brachytherapy. They reported similar local recurrence rates, disease-free and overall survivals in the two groups;[133]
- Another group compared results from wedge resection with and without brachytherapy delivered by placement of a radioactive mesh at the resection margin. There was no difference in morbidity, mortality or survival but there was a decrease in local recurrence in the group that received the mesh (19 vs 2%);[134]
- A different group reported the results of 48 patients who underwent wedge resection and brachytherapy delivered through three catheters placed at the resection margin at the time of surgery. Two patients had local recurrence over variable follow-up times. The authors felt the technique performed well from a safety standpoint;[135]
- Location of the segmentectomy and resection margins were reported to influence the rate of local recurrence. Resection of segments within the S1–3 region had higher rates of recurrence.[136]
Guidelines
The ACCP guidelines state that in patients with very poor lung function and a lung cancer in an area of upper lobe emphysema, it is recommended that combined lung volume reduction surgery and lung cancer resection be considered if both the FEV1 and the DLCO are more than 20% predicted.
The ERS/ESTS guidelines state that anatomical lobectomy with or without complementary LVRS should be performed in well-selected COPD patients with lung cancer. The ERS/ESTS guidelines also state that anatomical segmentectomy could be recommended in the following situations:
- Stage IA (tumor size 2–3 cm) that has margins of resection over 1 cm;
- Stage I in patients with poor lung function;
- Lung resection after prior lobectomy.
ERS/ESTS: wedge resection could be recommended in the following situations:
- Stage IA (tumor size < 2 cm);
- Small peripheral adenocarcinoma with an air-containing image (ground glass opacity) on high-resolution CT scan.
Perioperative Considerations
Evidence
Level of Care Patients who undergo resection for lung cancer at hospitals performing large numbers of such procedures have fewer perioperative deaths and survive longer than those whose surgery is performed at hospitals with a low volume.[2,137] Patients who see physicians with a higher volume are more likely to have their cancers histologically confirmed and to receive active treatment for their cancer.[138] Patients who are diagnosed by or referred to a specialist within 6 months of diagnosis have been shown to have a lower risk of death.[139] In-hospital mortality postlung resection is lower at teaching hospitals than nonteaching hospitals, independent of patient volume.[9] The establishment of a multidisciplinary lung cancer team at a single center resulted in more patients with inoperable non-small cell carcinoma receiving active treatment and a prolonged survival when compared with results from immediately prior to the team being established.[140]
Guidelines
The ACCP guidelines recommended that patients with lung cancer be assessed for curative surgical resection by a multidisciplinary team, which includes a thoracic surgeon specializing in lung cancer, a medical oncologist, a radiation oncologist and a pulmonologist.
The ERS/ESTS guidelines state that the management of lung cancer patients must be performed by multidisciplinary teams (a thoracic surgeon specializing in lung cancer, a medical oncologist, a radiation oncologist and a pulmonologist). The ERS/ESTS guidelines also state that the surgical treatment of lung cancer patients must be performed in specialized centers by qualified thoracic surgeons, since specialization has been shown to have a positive impact on respectability, postoperative mortality and long-term survival. The ERS/ESTS guidelines then say that surgical volume has been shown to have a positive impact on respectability, postoperative mortality and long-term survival. Lung cancer surgery should be performed in centers with an adequate volume of cases (although volume thresholds reported in the literature varied in size and definition, a minimum surgical volume of 20–25 major lung resections per year, lobectomy or pneumonectomy, should be advised).
Evidence
Smoking Cessation Current and former smoking has been shown to be a risk factor for postoperative pulmonary complications.[141,142] A paper from the cardiac surgery literature found that the surgical candidate needed to quit smoking 8 weeks prior to surgery to decrease the risk of pulmonary complications.[141] A second report of individuals undergoing a variety of surgeries found that a reduction of the amount smoked near the time of the surgery led to an increased risk of pulmonary complications.[142] A few reports are available from the thoracotomy literature. One study found that individuals who continue to smoke within 1 month of a pneumonectomy are at increased risk for developing major pulmonary events.[143] Another study was unable to find a paradoxical increase in pulmonary complications among those who quit smoking within 2 months of undergoing thoracotomy.[144] The sooner one is able to quit, the more likely it is that he or she will remain abstinent after surgery.[145]
Ancillary Care There is no direct evidence to support an additional role for bronchodilators and antibiotics in the lung resection candidate beyond what would be considered standard use for COPD or asthma. Little evidence exists to support the use of anti-inflammatory medications in the perioperative period. One report suggested that corticosteroid treatment suppresses cytokine production in resected lung specimens studied in vitro.[146] A second report suggested that administering clarithromycin prior to and after surgery leads to a reduction in clinical features of the systemic inflammatory response syndrome.[147] Traditional outcome measures, such as complications and mortality, could not be commented on.
Inspiratory muscle training and the use of incentive spirometry before and after resection have been reported to decrease the risk of postoperative pulmonary complications and to improve lung function outcomes.[148,149] A report of short-term noninvasive ventilation after lung resection showed improvement in oxygenation without worsening air leaks.[150] The effect of this intervention on other major complications was not reported. A separate group randomized 32 patients with a FEV1 less than 70% predicted who were scheduled for a lobectomy for lung cancer to noninvasive pressure support ventilation for 7 days prior to (1 h five-times daily) and 3 days after resection. They found improved FEV1, FVC, partial pressure of arterial oxygen (PaO2) and shorter hospital stays in the intervention group.[151] The use of thoracic epidural analgesia through the postoperative period has been associated with fewer respiratory complications (OR: 0.6) and a lower 30-day mortality.[42]
Perioperative Pulmonary Rehabilitation A report of eight patients who were denied resection based on poor lung function but then underwent 4 weeks of intensive inpatient pulmonary rehabilitation demonstrated that all eight were able to improve measures of lung function and exercise tolerance enough to permit the resection to occur. All survived resection, with only one requiring long-term oxygen therapy.[152] Another group identified lobectomy candidates with COPD who had a VO2 max less than 15 ml/kg/min. A total of 12 such subjects were enrolled in 4 weeks of preoperative rehabilitation. Standard measures of lung function did not change but the VO2 max increased by 2.8 ml/kg/min on average. The group had acceptable surgical morbidity and no deaths.[153] A study of ten patients with an FEV1 55% predicted, DLCO of 45% and significant limitation after resection found that 8 weeks of multidisciplinary inpatient rehabilitation led to improvement in the 6-min walk distance by 43.2% and exercise capacity by 34.4%, without a change in standard measures of pulmonary function.[154] Another group studied 618 individuals undergoing lung resection, 211 of whom were eligible for inpatient pulmonary rehabilitation.[155] A total of 25 patients agreed to participate in the 4-week program, and the other 186 were used as controls. Those who participated had poorer lung function at baseline. Rehabilitation took place 3 h per day, 5 days per week. Significant gains in the Borg dyspnea scale and 6-min walk distance were realized in the treated subjects. Their lung function was stable compared with baseline values. The control group deteriorated in all measures when taken 1 month postresection. The differences between the treated and control groups that existed at baseline were no longer present at the end of training.
Guidelines
The ACCP guidelines recommended that all patients with lung cancer be counseled regarding smoking cessation.
The ERS/ESTS guidelines state that smoking cessation of sufficient duration (2–4 weeks) before surgery should be recommended, since it may change the smoking behavior perioperatively and decrease postoperative complications. The ERS/ESTS guidelines also state that early pre- and postoperative rehabilitation should be recommended, since it may produce functional benefits in resectable lung cancer patients. Candidate selection, late outcomes (i.e., postoperative complications and death), and program content and duration need to be further investigated.
Conclusion
This article has detailed the rationale for pursuing a detailed pulmonary evaluation for potential lung resection candidates. There is an extensive amount of literature available to help guide us, as well as two recent sets of published guidelines.[25,26] As is highlighted by the differences within these guidelines, your approach to an individual patient should be based on your understanding of the available literature, your sense of your patient’s risk tolerance and knowledge of the strengths of your lung cancer team.
Expert Commentary
The decision to recommend lung resection as curative intent therapy for a patient with localized lung cancer can be a difficult one. There is a substantial body of literature available to help us predict someone’s risk of complications or mortality related to the cancer and/or the treatment. Two recent sets of guidelines help to summarize the available literature and put it into context. Despite this, there are very few absolute indicators of safety or excessive risk. Thus, many factors need to be considered when making a decision with an individual patient whose lung function is borderline, based on the previous literature and guidelines. I consider some of the following. Are there other options with more acceptable risk to benefit profiles? What type of risk tolerance does my patient have? What testing and treatment options are available in your area, and what are the strengths of my lung cancer team?
At present, in my clinic, I use the ACCP guidelines as a framework for my evaluation then individualize decisions with my patient’s characteristics and wishes in mind. I often do get both an FEV1 and DLCO as the initial testing both because I feel they are important and it is most practical to test them together. I believe the evidence is not strong enough to support the position of cardiopulmonary exercise testing within the ERS/ESTS guidelines. To simplify matters even further, one can focus on three numbers. First is 80% – if the FEV1 and DLCO are above 80% predicted then additional testing is not required. Second is 40% – if the ppoFEV1 or ppoDLCO is below 40%, then exercise testing should be performed. Third is 10 – if the VO2 max or its equivalent is below 10 ml/kg/min then alternative strategies for treatment should be discussed.
Recent advances have provided us with other options. Advances in perioperative support, sublobar resections, stereotactic body radiotherapy and radiofrequency ablation have provided us with options to discuss with our patients. Although the exact risks and benefits of these treatment modalities require clarification, they provide an opportunity to remain curative in our therapeutic intent in situations where we previously had only poor alternatives to surgery. Individual patients will have different tolerances to the risks and benefits of any approach that is outlined to them. One patient may consider a slightly higher cure rate worth the risk of a potentially lower postoperative activity tolerance, while another may not.
Advances that occur in our ability to predict functional outcomes, in surgical techniques, perioperative care, as well as pre- and postoperative medical and wellness management will continue to shift the thresholds that are used to assess the risks related to resection. Advances in testing related to early diagnosis, molecular prognosis and prediction of response to therapies will allow us to better predict the benefits of our chosen treatment plan. The final decision will always be made at the level of the individual patient.
Five-year View
In the next 5 years, several advances will occur that could influence our ability to judge the risks and benefits of lung resection. Additional tests of cardiopulmonary fitness whose predictive abilities could be validated include steady-state cardiopulmonary exercise testing, the impact of hyperinflation and air trapping on outcomes, the evaluation of daily physical activity, and DLCO changes with exertion. Preoperative sputum and exhaled gas analysis may influence perioperative treatment decisions in an attempt to mitigate risks. Imaging advances may allow us to more accurately predict postoperative lung function. Usable indices will be developed to help us predict immediate and delayed lung function changes as well as complications. The risks of resection will slowly decline as minimally invasive resections become more common and perioperative management advances become more generalized. We will gain knowledge about the true risks and benefits of alternatives to anatomical resections, such as sublobar resections (with and without locally delivered radiotherapy), stereotactic body radiotherapy and radiofrequency ablation. We will learn how to assess the nature of each individual’s lung cancer, allowing us to apply the most aggressive therapies more selectively. We will have more tools to allow us to have personalized discussions about the appropriate selection of treatment for each of our patients.
Sidebar
Key Issues
- There is a poor prognosis for lung cancer when surgery is not an option, a reasonable morbidity and mortality related to standard resection despite an ill population, and a modest decline in lung function and exercise capacity from resection.
- Lung resection should not be denied on the basis of age alone.
- The forced expiratory volume in 1 s and diffusing capacity for carbon monoxide are measures of pulmonary function most commonly used to assess someone’s ability to tolerate resection.
- There are several methods available to predict postoperative lung function. Most tend to underestimate actual postoperative lung function.
- Exercise testing can be used to help determine who may tolerate lung resection.
- Guidelines and testing algorithms are available to help you incorporate pulmonary function and exercise testing into decisions regarding patient’s ability to tolerate standard lung resection.
- Alternatives to standard lung resection, including lung volume reduction surgery, sublobar resections, stereotactic body radiotherapy and radiofrequency ablation, are available. Our understanding of the outcomes, risks and benefits of these standard resection alternatives is evolving.
References
- Damhuis RAM, Schutte PR. Resection rates and postoperative mortality in 7,899 patients with lung cancer. Eur. Respir. J. 9, 7–10 (1996).
- Little AG, Rusch VW, Bonner JA et al. Patterns of surgical care of lung cancer patients. Ann. Thorac. Surg. 80, 2051–2056 (2005).
- Baser S, Shannon VR, Eapen GA et al. Pulmonary dysfunction as a major cause of inoperability among patients with non-small-cell lung cancer. Clin. Lung Cancer 7, 344–349 (2006).
- Sobue T, Suzuki T, Matsuda M et al. Survival for clinical stage I lung cancer not surgically treated. Comparison between screen-detected and symptom-detected cases. The Japaneses Lung Cancer Screening Research Group. Cancer 69, 685–692 (1992).
- Motohiro A, Ueda H, Komatsu H et al. Prognosis of non-surgically treated, clinical stage I lung cancer patients in Japan. Lung Cancer 36, 65–69 (2002).
- Sato M, Saito Y, Endo C et al. The natural history of radiographically occult bronchogenic squamous cell carcinoma. A retrospective study of overdiagnosis bias. Chest 126, 108–113 (2004).
- Loewen GM, Watson D, Kohman L et al. Preoperative exercise noninvasive measurement for lung resection candidates: results of Cancer and Leukemia Group B protocol 9238. J. Thorac. Oncol. 2, 619–625 (2007).
- Allen MS, Darling GE, Pechet TV et al. Morbidity and mortality of major pulmonary resections in patients with early-stage lung cancer: initial results of the randomized, prospective ACOSOG Z0030 trial. Ann. Thorac. Surg. 81, 1013–1020 (2006).
- Meguid RA, Brooke BS, Chang DC, Sherwood JT, Brock MV, Yang SC. Are surgical outcomes for lung cancer resections improved at teaching hospitals? Ann. Thorac. Surg. 85, 1015–1025 (2008).
- Memtsoudis SG, Besculides MC, Zellos L, Patil N, Rogers SO. Trends in lung surgery. United States 1988 to 2002. Chest 130, 1462–1470 (2006).
- Boffa DJ, Allen MS, Grab JD, Gaissert HA, Harpole DH, Wright CD. Data from The Society of Thoracic Surgeons General Thoracic Surgery database: the surgical management of primary lung tumors. J. Thorac. Cardiovasc. Surg. 135, 247–254 (2008).
• Describes the population of patients presenting for resection and modern operative morbidity and mortality in expert hands.
- Wright CD, Henning AG, Grab JD, O’Brien SM, Peterson ED, Allen MS. Predictors of prolonged length of stay after lobectomy for lung cancer: a Society of Thoracic Surgeons General thoracic Surgery database risk-adjustment model. Ann. Thorac. Surg. 85, 1857–1865 (2008).
- Schussler O, Alifano M, Dermine H et al. Postoperative pneumonia after major lung resection. Am. J. Respir. Crit. Care Med. 173, 1161–1169 (2006).
- Harpole DH, Liptay MJ, DeCamp MM et al. Prospective analysis of pneumonectomy: risk factors for major morbidity and cardiac dysrhythmias. Ann. Thorac. Surg. 61, 977–982 (1996).
- Dales RE, Dionne G, Leech JA et al. Preoperative prediction of pulmonary complications following thoracic surgery. Chest 104, 155–159 (1993).
- Duque JL, Ramos G, Castrodeza J et al. Early complications in surgical treatment of lung cancer: a prospective, multicenter study. Ann. Thorac. Surg. 63, 944–950 (1997).
- Bolliger CT, Jordan P, Soler M et al. Pulmonary function and exercise capacity after lung resection. Eur. Respir. J. 9, 415–421 (1996).
- Nezu K, Kushibe K, Tojo T, Takahama M, Kitamura S. Recovery and limitation of exercise capacity after lung resection for lung cancer. Chest 113, 1511–1516 (1998).
- Bolliger CT, Guckel C, Engel H et al. Prediction of functional reserves after lung resection: comparison between quantitative computed tomography, scintigraphy, and anatomy. Respiration 69, 482–489 (2002).
• Compares methods used to predict postoperative pulmonary function. It suggests good results for most methods for lobectomy and better estimation with perfusion imaging for pneumonectomy.
- Brunelli A, Xiume F, Refai M et al. Evaluation of expiratory volume, diffusion capacity, and exercise tolerance following major lung resection. A prospective follow-up analysis. Chest 131, 141–147 (2007).
- Smulders SA, Smeenk WJM, Janssen-Heijnen MLG, Postmus PE. Actual and predicted postoperative changes in lung function after pneumonectomy. A retrospective analysis. Chest 125, 1735–1741 (2004).
- Edwards JG, Duthie DJR, Waller DA. Lobar volume reduction surgery: a method of increasing the lung cancer resection rate in patients with emphysema. Thorax 56, 791–795 (2001).
- Bobbio A, Chetta A, Carbognani P et al. Changes in pulmonary function test and cardio-pulmonary exercise capacity in COPD patients after lobar pulmonary resection. Eur. J. Cardiothorac. Surg. 28, 754–758 (2005).
- Brunelli A, Socci L, Refai M, Salati M, Xiume F, Sabbatini A. Quality of life before and after major lung resection for lung cancer: a prospective follow-up analysis. Ann. Thorac. Surg. 84, 410–416 (2007).
• One of few articles that has looked at the quality of life after lung resection. It suggests little change after recovery and a lack of association between quality-of-life measures and pulmonary function measures.
- Collice GL, Shafazand S, Griffin JP, Keenan R, Bolliger CT. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 132, 161–177 (2007).
•• Most recent edition of the guidelines for the evaluation of patients prior to lung cancer resection from the American College of Chest Physicians.
- Brunelli A, Charloux A, Bolliger CT et al. ERS/ESTS clinical guidelines on fitness for radical therapy in lung cancer patients (surgery and chemo-radiotherapy). Eur. Respir. J. 34, 17–41 (2009).
•• Guidelines for the evaluation of patients prior to lung cancer resection from the European Respiratory Society and European Society of Thoracic Surgeons.
- Brown JS, Eraut D, Trask C, Davison AG. Age and the treatment of lung cancer. Thorax 51, 564–568 (1996).
- Kirsh MM, Rotman H, Bove E et al. Major pulmonary resection for bronchogenic carcinoma in the elderly. Ann. Thorac. Surg. 22, 369–373 (1976).
- Breyer RH, Zippe C, Pharr WF et al. Thoracotomy in patients over age seventy years: ten-year experience. J. Thorac. Cardiovasc. Surg. 81, 187–193 (1981).
- Nagasaki F, Flehinger BJ, Martini N. Complications of surgery in the treatment of carcinoma of the lung. Chest 82, 25–29 (1982).
- Ginsberg RJ, Hill LD, Eagan RT et al. Modern thirty-day operative mortality for surgical resections in lung cancer. J. Thorac. Cardiovasc. Surg. 86, 654–658 (1983).
- Sherman S, Guidot CE. The feasibility of thoracotomy for lung cancer in the elderly. JAMA 258, 927–930 (1987).
- Ishida T, Yokoyama H, Kaneko S et al. Long-term results of operation for non-small cell lung cancer in the elderly. Ann. Thorac. Surg. 50, 919–922 (1990).
- Shirakusa T, Tsutsui M, Iriki N et al. Results of resection for bronchogenic carcinoma in patients over the age 80. Thorax 44, 189–191 (1989).
- Roxburgh JC, Thompson J, Goldstraw P. Hospital mortality and long-term survival after pulmonary resection in the elderly. Ann. Thorac. Surg. 51, 800–803 (1991).
- Riquet M, Manac’h D, Pimpec-Barthes FL et al. Operation for lung cancer in the elderly: what about octogenarians? Ann. Thorac. Surg. 58, 916 (1994).
- Massard G, Moog R, Wihlm JM et al. Thorac. Cardiovasc. Surg. 44, 40–45 (1996).
- Pagni S, Federico JA, Ponn RB. Pulmonary resection for lung cancer in octogenarians. Ann. Thorac. Surg. 63, 785–789 (1997).
- Port JL, Kent M, Korst RJ et al. Surgical resection for lung cancer in the octogenarian. Chest 126, 733–738 (2004).
- Brock MV, Kim MP, Hooker CM et al. Pulmonary resection in octogenarians with stage I nonsmall cell lung cancer: a 22-year experience. Ann. Thorac. Surg. 77, 271–277 (2004).
- Birim O, Zuydendorp HM, Maat APW, Kappetein AP, Eijkemans MJC, Bogers AJJC. Lung resection for non-small-cell lung cancer in patients older than 70: mortality, morbidity, and late survival compared with the general population. Ann. Thorac. Surg.76(6),1796–801 (2003).
- Licker MJ, Widdiker I, Robert J et al. Operative mortality and respiratory complications after lung resection for cancer: impact of chronic obstructive pulmonary disease and time trends. Ann. Thorac. Surg. 81, 1830–1838 (2006).
- Boushy SF, Billig DM, North LB, Helgason AH. Clinical course related to preoperative and postoperative pulmonary function in patients with bronchogenic carcinoma. Chest 59, 383–391 (1971).
- Wernly JA, DeMeester TR, Kirchner PT et al. Clinical value of quantitative ventilation-perfusion lung scans in the surgical management of bronchogenic carcinoma. J. Thorac. Cardiovasc. Surg. 80, 535–543 (1980).
- Miller JI. Physiologic evaluation of pulmonary function in the candidate for lung resection. J. Thorac. Cardiovasc. Surg. 105, 347–352 (1993).
- Wyser C, Stulz P, Soler M et al. Prospective evaluation of an algorithm for the functional assessment of lung resection candidates. Am. J. Respir. Crit. Care Med. 159, 1450–1456 (1999).
- Markos J, Mullan BP, Hillman DR et al. Preoperative assessment as a predictor of mortality and morbidity after lung resection. Am. Rev. Respir. Dis. 139, 902–910 (1989).
- Ferguson MK, Little L, Rizzo L et al. Diffusing capacity predicts morbidity and mortality after pulmonary resection. J. Thorac. Cardiovasc. Surg. 96, 894–900 (1988).
- Wang J, Olak J, Ultmann RE, Ferguson MK. Assessment of pulmonary complications after lung resection. Ann. Thorac. Surg. 67, 1444–1447 (1997).
- Bousamra M, Presberg KW, Chammas JH et al. Early and late morbidity in patients undergoing pulmonary resection with low diffusion capacity. Ann. Thorac. Surg. 62, 968–975 (1996).
- Brunelli A, Al Refai M, Salati M, Sabbatini A, Morgan-Hughes NJ, Rocco G. Carbon monoxide lung diffusion capacity improves risk stratification in patients without airflow limitation: evidence for systematic measurement before lung resection. Eur. J. Cardiothorac. Surg. 29, 567–570 (2006).
- Zeiher BG, Gross TJ, Kern JA et al. Predicting postoperative pulmonary function in patients undergoing lung resection. Chest 108, 68–72 (1995).
- Nakahara K, Monden Y, Ohno K et al. A method for predicting postoperative lung function and its relation to postoperative complications in patients with lung cancer. Ann. Thorac. Surg. 39, 260–265 (1985).
- Kristersson S, Lindell SE, Svanberg L. Prediction of pulmonary function loss due to pneumonectomy using 133Xe-radiospirometry. Chest 62, 694–698 (1972).
- Bria WF, Kanarek DJ, Kazemi H. Prediction of postoperative pulmonary function following thoracic operations: value of ventilation-perfusion scanning. J. Thorac. Cardiovasc. Surg. 86, 186–192 (1983).
- Ali MK, Mountain CF, Ewer MS et al. Predicting loss of pulmonary function after pulmonary resection for bronchogenic carcinoma. Chest 77, 337–342 (1980).
- Corris PA, Ellis DA, Hawkins T, Gibson GJ. Use of radionuclide scanning in the preoperative estimation of pulmonary function after pneumonectomy. Thorax 42, 285–291 (1987).
- Ladurie MLR, Ranson-Bitker B. Uncertainties in the expected value for forced expiratory volume in one second after surgery. Chest 90, 222–228 (1986).
- Giordano A, Calcagni ML, Meduri G et al. Perfusion lung scintigraphy for the prediction of postlobectomy residual pulmonary function. Chest 111, 1542–1547 (1997).
- Wu MT, Chang JM, Chiagn AA et al. Use of quantitative CT to predict postoperative lung function in patients with lung cancer. Radiology 191, 257–262 (1994).
- Wu MT, Pan HB, Chiang AA et al. Prediction of postoperative lung function in patients with lung cancer: comparison of quantitative CT with perfusion scintigraphy. AJR Am. J. Roentgenol. 178, 667–672 (2002).
- Sverzellati N, Chetta A, Calabro E et al. Reliability of quantitative computed tomography to predict postoperative lung function in patients with chronic obstructive pulmonary disease having a lobectomy. J. Comput. Assist. Tomogr. 29, 819–824 (2005).
- Ueda K, Kaneda Y, Sudoh M et al. Role of quantitative CT in predicting hypoxemia and complications after lung lobectomy for cancer, with special reference to area of emphysema. Chest 128, 3500–3506 (2005).
- Kearney DJ, Lee TH, Reilly JJ et al. Assessment of operative risk in patients undergoing lung resection: importance of predicted pulmonary function. Chest 105, 753–759 (1994).
- Mitsudomi T, Mizoue T, Yoshimatsu T et al. Postoperative complications after pneumonectomy for treatment of lung cancer: multivariate analysis. J. Surg. Oncol. 61, 218–222 (1996).
- Ribas J, Diaz O, Barbera JA et al. Invasive exercise testing in the evaluation of patients at high-risk for lung resection. Eur. Respir. J. 12, 1429–1435 (1998).
- Nakahara K, Ohno K, Hashimoto J et al. Prediction of postoperative respiratory failure in patients undergoing lung resection for lung cancer. Ann. Thorac. Surg. 46, 549–552 (1988).
- Brunelli A, Fianchini A. Predicted postoperative FEV1 and complications in lung resection candidates. Chest 111, 1145–1146 (1997).
- Putnam JB, Lammermeier DE, Colon R et al. Predicted pulmonary function and survival after pneumonectomy for primary lung carcinoma. Ann. Thorac. Surg. 49, 909–915 (1990).
- Wahi R, McMurtrey MJ, DeCaro LF et al. Determinants of perioperative morbidity and mortality after pneumonectomy. Ann. Thorac. Surg. 48, 33–37 (1989).
- Boysen PG, Block AJ, Olsen GN et al. Prospective evaluation for pneumonectomy using the 99mTechnetium quantitative perfusion lung scan. Chest 72, 422–425 (1977).
- Boysen PG, Harris JO, Block AJ, Olsen GN. Prospective evaluation of pneumonectomy using perfusion scanning: follow-up beyond one year. Chest 80, 163–166 (1981).
- Ferguson MK, Reeder LB, Mick R. Optimizing selection of patients for major lung resection. J. Thorac. Cardiovasc. Surg. 109, 275–283 (1995).
- Ferguson MK, Vigneswaran WT. Diffusing capacity predicts morbidity after lung resection in patients without obstructive lung disease. Ann. Thorac. Surg. 85, 1158–1165 (2008).
- Santini M, Fiorello A, Vicidomini G, Di Crescenzo VG, Laperuta P. Role of diffusing cpacity in predicting complications after lung resection for cancer. Thorac. Cardiovasc. Surg. 55, 391–394 (2007).
- Pierce R, Copland JM, Sharpe K, Barter CE. Preoperative risk evaluation for lung cancer resection: Predicted postoperative product as a predictor of surgical mortality. Am. J. Respir. Crit. Care Med. 150, 947–955 (1994).
- Morice RC, Peters EJ, Ryan MB et al. Exercise testing in the evaluation of patients at high risk for complications from lung resection. Chest 101, 356–361 (1992).
- Walsh GL, Morice RC, Putnam JB et al. Resection of lung cancer is justified in high-risk patients selected by exercise oxygen consumption. Ann. Thorac. Surg. 58, 704–711 (1994).
- Pate P, Tenholder MF, Griffin JP et al. Preoperative assessment of the high-risk patient for lung resection. Ann. Thorac. Surg. 61, 1494–1500 (1996).
- Olsen GN, Weiman DS, Bolton JWR et al. Submaximal invasive exercise testing and quantitative lung scanning in the evaluation for tolerance of lung resection. Chest 95, 267–273 (1989).
- Bolliger CT, Wyser C, Roser H et al. Lung scanning and exercise testing for the prediction of postoperative performance in lung resection candidates at increased risk for complications. Chest 108, 341–348 (1995).
- Bolliger CT, Jordan P, Soler M et al. Exercise capacity as a predictor of postoperative complications in lung resection candidates. Am. J. Respir. Crit. Care Med. 151, 1472–1480 (1995).
- Larsen KR, Svendsen UG, Milman N et al. Exercise testing in the preoperative evaluation of patients with bronchogenic carcinoma. Eur. Respir. J. 10, 1559–1565 (1997).
- Brutsche MH, Spiliopoulos A, Bolliger CT et al. Exercise capacity and extent of resection as predictors of surgical risk in lung cancer. Eur. Respir. J. 15, 828–832 (2000).
- Win T, Jackson A, Sharples L et al. Cardiopulmonary exercise tests and lung cancer surgical outcome. Chest 127, 1159–1165 (2005).
- Benzo R, Kelley GA, Recchi L, Hofman A, Sciurba F. Complications of lung resection and exercise capacity: a meta-analysis. Respir. Med. 101, 1790–1797 (2007).
• Provides a good summary of studies that have looked at the value of cardiopulmonary exercise testing in the preoperative evaluation of lung cancer patients.
- Brunelli A, Belardinelli R, Refai M et al. Peak oxygen consumption during cardiopulmonary exercise test improves risk stratification in candidates to major lung resection. Chest 135, 1260–1267 (2009).
• Describes the role of cardiopulmonary exercise testing as an upfront test for those undergoing lung cancer resection. It suggests the test is underused.
- Nakagawa K, Nakahara K, Miyoshi S, Kawashima Y. Oxygen transport during incremental exercise load as a predictor of operative risk in lung cancer patients. Chest 101, 1369–1375 (1992).
- Wang JS, Abboud RT, Evans KG et al. Role of CO diffusing capacity during exercise in the preoperative evaluation for lung resection. Am. J. Respir. Crit. Care Med. 162, 1435–1444 (2000).
- Rao V, Todd TRJ, Kuus A et al. Exercise oximetry versus spirometry in the assessment of risk prior to lung resection. Ann. Thorac. Surg. 60, 603–609 (1995).
- Ninan M, Sommers KE, Landreneau RJ et al. Standardized exercise oximetry predicts postpneumonectomy outcome. Ann. Thorac. Surg. 64, 328–333 (1997).
- Win T, Jackson A, Groves AM et al. Relationship of shuttle walk test and lung cancer surgical outcome. Eur. J. Cardiothorac. Surg. 26, 1216–1219 (2004).
- Bolton JWR, Weiman DS, Haynes JL et al. Stair climbing as an indicator of pulmonary function. Chest 92, 783–788 (1987).
- Pollock M, Roa J, Benditt J, Celli B. Estimation of ventilatory reserve by stair climbing: a study in patients with chronic airflow obstruction. Chest 104, 1378–1383 (1993).
- Olsen GN, Bolton JWR, Weiman DS, Hornung CA. Stair climbing as an exercise test to predict the postoperative complications of lung resection: two years’ experience. Chest 99, 587–590 (1991).
- Holden DA, Rice TW, Stelmach K, Meeker DP. Exercise testing, 6-min walk, and stair climb in the evaluation of patients at high risk for pulmonary resection. Chest 102, 1774–1779 (1992).
- Brunelli A, Al Refai M, Monteverde M et al. Stair climbing test predicts cardiopulmonary complications after lung resection. Chest 121, 1106–1110 (2002).
- Brunelli A, Refai M, Xiume F et al. Performance at symptom-limited stair-climbing test is associated with increased cardiopulmonary complications, mortality, and costs after major lung resection. Ann. Thorac. Surg. 86, 240–248 (2008).
- Brunelli A, Sabbatini A, Xiume F et al. Inability to perform maximal stair climbing test before lung resection: a propensity score analysis on early outcome. Eur. J. Cardiothorac. Surg. 27, 367–372 (2005).
- Singh SJ, Morgan MDL, Scott S et al. Development of a shuttle walking test of disability in patients with chronic airways obstruction. Thorax 47, 1019–1024 (1992).
- Singh SJ, Morgan MDL, Hardman AE et al. Comparison of oxygen uptake during a conventional treadmill test and the shuttle walking test in chronic airflow limitation. Eur. Respir. J. 7, 2016–2020 (1994).
- Turna A, Mercan CA, Bedirhan MA. Prediction of morbidity after lung resection in patients with lung cancer using fuzzy logic. Thorac. Cardiovasc. Surg. 53, 368–374 (2005).
- Olsen GN, Block AJ, Swenson EW et al. Pulmonary function evaluation of the lung resection candidate: a prospective study. Am. Rev. Respir. Dis. 111, 379–387 (1975).
- Geddes D, Davies M, Koyama H et al. Effect of lung-volume-reduction surgery in patients with severe emphysema. N. Engl. J. Med. 343, 239–245 (2000).
- National Emphysema Treatment Trial Research Group. Patients at high risk of death after lung-volume-reduction surgery. N. Engl. J. Med. 345, 1075–1083 (2001).
- National Emphysema Treatment Trial Research Group. A randomized trial comparing lung volume-reduction surgery with medical therapy for severe emphysema. N. Engl. J. Med. 348, 2059–2073 (2003).
- Rozenshtein A, White CS, Austin JHM et al. Incidental lung carcinoma detected at CT in patients selected for lung volume reduction surgery to treat severe pulmonary emphysema. Radiology 207, 487–490 (1998).
- Choong CK, Meyers BF, Battafarano RJ et al. Lung cancer resection combined with lung volume reduction in patients with severe emphysema. J. Thorac. Cardiovasc. Surg. 127, 1323–1331 (2004).
- DeRose JJ, Argenziano M, El-Amir N et al. Lung reduction operation and resection of pulmonary nodules in patients with severe emphysema. Ann. Thorac. Surg. 65, 314–318 (1998).
- DeMeester SR, Patterson GA, Sundaresan RS, Cooper JD. Lobectomy combined with volume reduction for patients with lung cancer and advanced emphysema. J. Thorac. Cardiovasc. Surg. 115, 681–688 (1998).
- Ojo TC, Martinez F, Paine R et al. Lung volume reduction surgery alters management of pulmonary nodules in patients with severe COPD. Chest 112, 1494–1500 (1997).
- McKenna RJ, Fischel RJ, Brenner M, Gelb AF. Combined operations for lung volume reduction surgery and lung cancer. Chest 110, 885–888 (1996).
- Pompeo E, Dominicis E, Ambrogi V et al. Quality of life after tailored combined surgery for stage I non-small-cell lung cancer and severe emphysema. Ann. Thorac. Surg. 76, 1821–1827 (2003).
- Lung Cancer Study Group. Randomized trial of lobectomy versus limited resection for T1N0 non-small cell lung cancer. Ann. Thorac. Surg. 60, 615–623 (1995).
• This paper is most often quoted when suggesting lobectomy outperforms sublobar resections.
- Lizasa T, Suzuki M, Yasufuku et al. Preoperative pulmonary function as a prognostic factor for stage I non-small cell lung carcinoma. Ann. Thorac. Surg. 77, 1896–1903 (2004).
- Mery CM, Pappas AN, Bueno R et al. Similar long-term survival of elderly patients with non-small cell lung cancer treated with lobectomy or wedge resection withing the surveillance, epidemiology, and end results database. Chest 128, 237–245 (2005).
- Okada M, Nishio W, Sakamoto T et al. Effect of tumor size on prognosis in patients with non-small cell lung cancer: the role of segmentectomy as a type of lesser resection. J. Thorac. Cardiovasc. Surg. 129, 87–93 (2005).
- Martin-Ucar AE, Nakas A, Pilling JE, West KJ, Waller DA. A case-matched study of anatomical segmentectomy versus lobectomy for stage I lung cancer in high-risk patients. Eur. J. Cardiothorac. Surg. 27, 675–679 (2005).
- El-Sherif A, Gooding WE, Santos R et al. Outcomes of sublobar resection versus lobectomy for stage I non-small cell lung cancer: a 13-year analysis. Ann. Thorac. Surg. 82, 408–416 (2006).
- Ghosh S, Sujendran V, Alexiou C, Beggs L, Beggs D. Long term results of surgery versus continuous hyperfractionated accelerated radiotherapy (CHART) in patients aged >70 years with stage I non-small cell lung cancer. Eur. J. Cardiothorac. Surg. 24, 1002–1007 (2003).
- Landreneau RJ, Sugarbaker DJ, Mack MJ et al. Wedge resection versus lobectomy for stage I (T1N0M0) non-small-cell lung cancer. J. Thorac. Cardiovasc. Surg. 113, 691–670 (1997).
- Yoshida J, Nagai K, Yokose T et al. Limited resection trial for pulmonary ground-glass opacity nodules: fifty-case experience. J. Thorac. Cardiovasc. Surg. 129, 991–996 (2005).
- Sienel W, Dango S, Kirschbaume A et al. Sublobar resections in stage IA non-small cell lung cancer: segmentectomies result in significantly better cancer-related survival than wedge resections. Eur. J. Cardiothorac. Surg. 33, 728–734 (2008).
- Griffin JP, Eastridge CE, Tolley EA, Pate JW. Wedge resection for non-small cell lung cancer in patients with pulmonary insufficiency: prospective ten-year survival. J. Thorac. Oncol. 1, 960–964 (2006).
- Kraev A, Rassias D, Vetto J et al. Wedge resection vs lobectomy. 10-year survival in stage I primary lung cancer. Chest 131, 136–140 (2007).
- Linden PA, Bueno R, Colson YL et al. Lung resection in patients with preoperative FEV1 < 35% predicted. Chest 127, 1984–1990 (2005).
- Koizumi K, Haraguchi S, Hirata T et al. Surgical treatment for lung cancer patients with poor pulmonary function. Ann. Thorac. Cardiovasc. Surg. 11, 87–92 (2005).
- Takizawa T, Haga M, Yagi N et al. Pulmonary function after segmentectomy for small peripheral carcinoma of the lung. J. Thorac. Cardiovasc. Surg. 118, 536–541 (1999).
- Keenan RJ, Landreneau RJ, Maley RH et al. Segmental resection spares pulmonary function in patients with stage I lung cancer. Ann. Thorac. Surg. 78, 228–233 (2004).
- Nugent AM, Steele IC, Carragher AM et al. Effect of thoracotomy and lung resection on exercise capacity in patients with lung cancer. Thorax 54, 334–338 (1995).
- Shennib H, Bogart J, Herndon JE et al. Video-assisted wedge resection and local radiotherapy for peripheral lung cancer in high-risk patients: the Cancer and Leukemia Group B (CALGB) 9335, a Phase II, multi-institutional cooperative group study. J. Thorac. Cardiovasc. Surg. 129, 813–818 (2005).
- Goldstein NS, Ferkowicz M, Kestin L, Chmielewski GW, Welsh RJ. Wedge resection margin distances and residual adenocarcinoma in lobectomy specimens. Am. J. Clin. Pathol. 120, 720–724 (2003).
- Birdas TJ, Koehler RPM, Colonias A et al. Sublobar resection with brachytherapy versus lobectomy for stage Ib nonsmall cell lung cancer. Ann. Thorac. Surg. 81, 434–439 (2006).
- Santos R, Colonias A, Parda D et al. Comparison between sublobar resection and 125 I brachytherapy following sublobar resection in high-risk patients with stage 1 non-small cell lung cancer. Surgery 134, 691–697 (2003).
- McKenna RJ, Mahtabifard A, Yap J et al. Wedge resection and brachytherapy for lung cancer in patients with poor pulmonary function. Ann. Thorac. Surg. 85, S733–S736 (2008).
- Sienel W, Stremmel C, Kirschbaum et al. Frequency of local recurrence following segmentectomy of stage IA non-small cell lung cancer is influenced by segment localization and width of resection margins – implications for patient selection for segmentectomy. Eur. J. Cardiothorac. Surg. 31, 522–528 (2007).
- Bach PB, Cramer LD, Schrag D, Downey RJ, Gelfand SE, Begg CB. The influence of hospital volume on survival after resection for lung cancer. N. Engl. J. Med. 345, 181–188 (2001).
• Highlights the improvement in outcomes with lung resection that result from having surgery in a high volume center.
- Muers MF, Haward RA. Management of lung cancer. Thorax 51, 557–560 (1996).
- Gregor A, Thomson CS, Brewster DH et al. Management and survival of patients with lung cancer in Scotland diagnosed in 1995: results of a national population based study. Thorax 56, 212–217 (2001).
- Forrest LM, McMillan DC, McArdle CS, Dunlop DJ. An evaluation of the impact of a multidisciplinary team, in a single center, on treatment and survival in patients with inoperable non-small-cell lung cancer. Br. J. Cancer 93, 977–978 (2005).
- Warner MA, Divertie MB, Tinker JH. Preoperative cessation of smoking and pulmonary complications in coronary artery bypass patients. Anesthesiology 60, 380–383 (1984).
- Bluman LG, Mosca L, Newman N, Simon DG. Preoperative smoking habits and postoperative pulmonary complications. Chest 113, 883–889 (1998).
- Vaporciyan AA, Merriman KW, Ece F et al. Incidence of major pulmonary morbidity after pneumonectomy: association with timing of smoking cessation. Ann. Thorac. Surg. 73, 420–426 (2002).
- Barrera R, Shi W, Amar D et al. Smoking and timing of cessation: impact on pulmonary complications after thoractomy. Chest 127, 1977–1983 (2005).
- Dresler CM, Bailey M, Roper CR, Patterson A, Cooper JD. Smoking cessation and lung resection. Chest 110, 1199–1202 (1996).
- Mitsuta K, Shimoda T, Fukushima C et al. Preoperative steroid therapy inhibits cytokine production in the lung parenchyma in asthmatic patients. Chest 120, 1175–1183 (2001).
- Hirata T, Ogawa E, Takenaka K, Kawashita F. Suppression of postoperative systemic inflammatory response syndrome with clarithromycin following lung cancer surgery. Eur. Surg. Res. 36, 13–19 (2004).
- Weiner P, Man A, Weiner M et al. The effect of incentive spirometry and inspiratory muscle training on pulmonary function after lung resection. J. Thorac. Cardiovasc. Surg. 113, 552–557 (1997).
- Algar FJ, Alvarez A, Salvatierra A, Baamonde C, Aranda JL, Lopez-Pujol FJ. Predicting pulmonary complications after pneumonectomy for lung cancer. Eur. J. Cardiothorac. Surg. 23, 201–208 (2003).
- Aguilo R, Togores B, Pons S, Rubi M, Barbe F, Agusti AGN. Noninvasive ventilatory support after lung resectional surgery. Chest 112, 117–121 (1997).
- Perrin C, Jullien V, Venissac N et al. Prophylactic use of noninvasive ventilation in patients undergoing lung resectional surgery. Respir. Med. 101, 572–578 (2007).
- Cesario A, Ferri L, Galetta D et al. Preoperative pulmonary rehabilitation and surgery for lung cancer. Lung Cancer57(1),118–119 (2007).
- Bobbio A, Chetta A, Ampollini L et al. Preoperative pulmonary rehabilitation in patients undergoing lung resection for non-small cell lung cancer. Eur. J. Cardiothorac. Surg. 33, 95–98 (2008).
- Spruit MA, Janssen PP, Willemsen SCP, Hochstenbag MMH, Wouters EFM. Exercise capacity before and after an 8-week multidisciplinary inpatient rehabilitation program in lung cancer patients: a pilot study. Lung Cancer 52, 257–260 (2006).
- Cesario A, Ferri L, Galetta D et al. Post-operative respiratory rehabilitation after lung resection for non-small cell lung cancer. Lung Cancer57(2),175–180 (2007).
- Evans EWT. Resection for bronchial carcinoma in the elderly. Thorax 28, 86–88 (1973).
- Smith TP, Kinasewitz GT, Tucker WY et al. Exercise capacity as a predictor of post-thoracotomy morbidity. Am. Rev. Respir. Dis. 129, 730–734 (1984).
- Bechard D, Wetstein L. Assessment of exercise oxygen consumption as preoperative criterion for lung resection. Ann. Thorac. Surg. 44, 344–349 (1987).
Papers of special note have been highlighted as:
• of interest
•• of considerable interest