Some of the videos are silly, cheesy even… But ugly track suits aside…
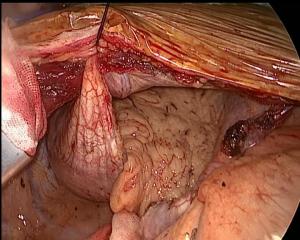
The results are, in arguably, wonderful. Patients eating, drinking, walking, and relaxing just an hour after major lung surgery.
Dr. Joao Carlos Das Neves Pereira is a Brazilian thoracic surgeon, who has been the primary author and leader on several articles, and programs for what he is calling ‘extreme fast track thoracic surgery’. He was also one of the featured speakers at International VATS 2018. “Better than before” is his model. “Patient empowerment’ is his ideology.
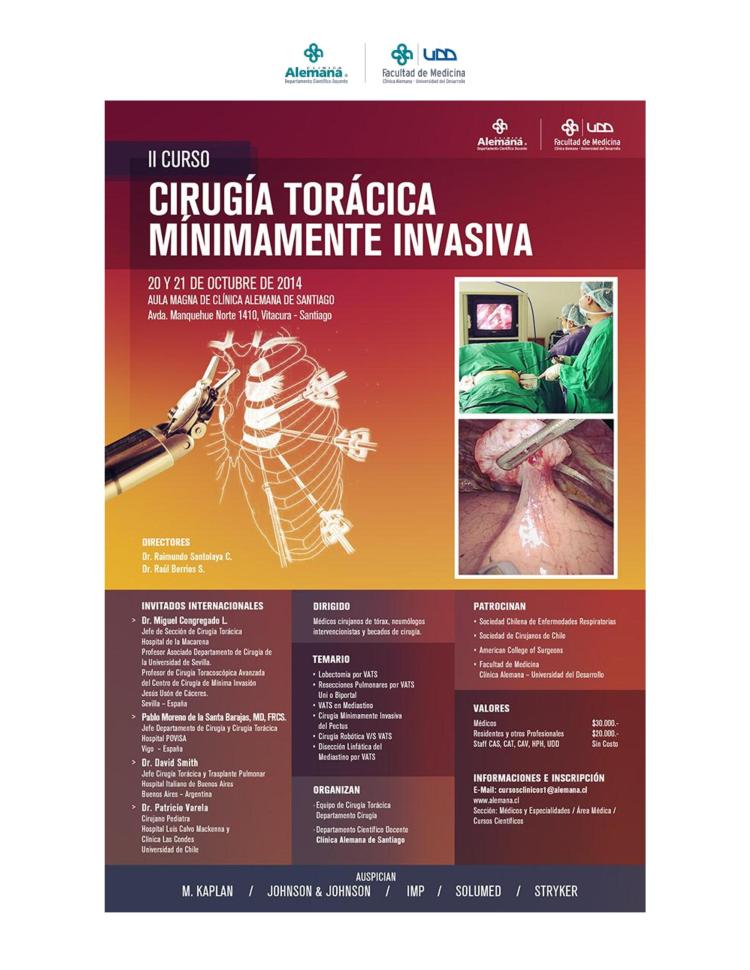
His presentation was easily the best in show, so to speak.. What’s more remarkable about his results are – that this isn’t new. He’s been doing it for more than a decade. In fact, he published an article on his experience in the European Journal of cardio-thoracic surgery was back in 2009. And now he is responsible for the implementation of a multi-disciplinary program at two hospitals on two continents – one on Paris, France and the second in Sao Paulo, Brazil.
So what does he do? How does he do it? And why aren’t the rest of us doing it?
What he does: “Feed & walk”
Change the existing surgical traditions:
- no prolonged fasting
- no cold operating rooms
- no IV opioids
He does this with a multifaceted program that starts several weeks before surgery; with a comprehensive nutrition, smoking cessation and and an exercise regimen.
The night before:
- Aromatherapy with lavender / Orange to promote sleep.
- Avoid benzodiazepines
On the morning of surgery
- patients are able to drink liquids within two hours of surgery, preventing dehydration and eliminating the need for IV fluids (no starving!)
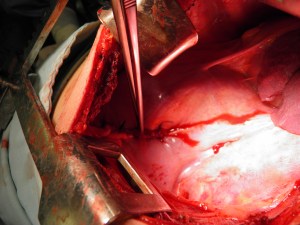
During surgery
- Normothermia
- Multi-modality approach for anxiety/ nausea/ vomiting / pain
- Opioid-free
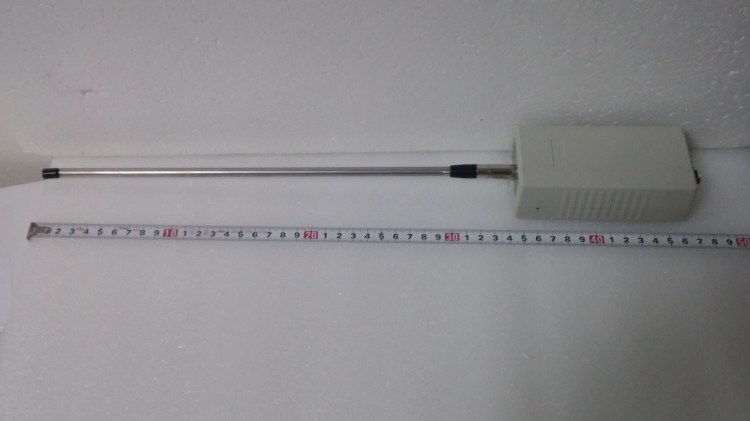
Patient analgesia and anesthetic is treated with a combination of approaches including hypnosis, pre-emptive oral medications, BIS for awake anesthesia, minimally invasive airways. Patients are only given very short acting medications such as ketamine, or propofol combined with local anesthesia. By avoiding narcotics, there is a reduction in both sedation, and GI complications post-operatively.
Patients who are able to readily wake up after surgery and who haven’t had narcotics that adversely affect bowel function) are able to eat and drink immediately after surgery.
Post-operative
- Immediate extubation (once the specimen is out of the chest)
- Immediate feeding
- Immediate exercise
- “Hands free” care: No IV lines, oral medications only, patient controlled and opioid free.
Patients are encouraged to wear their own clothing before going to the exercise room, the outside garden or walking the halls. Post-operative pain management consists of oral medications only, and is augmented by physical therapy, acupuncture, aromatherapy and massage. Friends and family are instructed in the proper massage techniques so that they are able to participate in the patients care (also shortage of massage therapists). Patient recovery is enhanced by conviviality: patients don’t spend time in the rooms, alone or in bed. Patients are welcome to spend time in open spaces, aromatherapy areas, exercise rooms, a japanese style garden, an indoor garden and a tea room. Patients are encouraged to socialize and spend time with other patients.
While some of these ideas are novel, there is no magic surgical technique, and no miracle drug to account for these results – which are arguably better the most of ours. But it’s not just aromatherapy, it’s a philosophy of care.
More importantly, what Dr. Das Neves Pereira and his colleagues have; that many of us find difficult to replicate – is patient buy-in. We can call it “Patient empowerment” but it’s the part that many of us continue to struggle with.
But Dr. Das Neves Pereira’s lecture leaves us with more questions as well as answers..
Would this work for your practice? And why aren’t the rest of us already doing it? Will the patients accept it?
For the answer to this – we have to look at our own practices, in the here and now, in late 2018. A recent issue of the thoracic journal of disease did just that, devoting an entire issue to ERAS (enhanced recovery and fast track programs) while providing blueprints for anesthesiologists, nursing and physical therapists. But for many of us, the pat and simple answer is something like this:
“While most of my patients wouldn’t mind some aromatherapy or a massage after surgery, the unfortunate truth is that few would participate in a pre-operative program stressing diet and exercise. Even fewer patients would sign on for a program that restricts narcotics. Many of us already know this about our patient populations because we try routinely to incorporate more holistic practices into our treatment in a daily basis. While holistic premises and alternative treatments make billions of dollars in the United States (under the guise of prevention) it’s still a culture that is highly dependent on fast, and immediate remedies and a strong belief that very little post-operative pain is acceptable or tolerable. For every one patient that would embrace the philosophies of extreme rehabilitation, there would be another 200 screaming at the nurses for IV dilaudid.”
Much of the research actually confirms this view:
British researchers, Rogers et al. (2018) had a similar experience, noting in their recent publication that benefits of enhanced recovery protocols were dependent on compliance (and adherence) to protocols – particularly in regards to pre-operative dietary modification, and early post-operative ambulation. Refai et al. (2018) have attempted to address these issues with a comprehensive patient education component. However, their publication does not address whether these interventions increased compliance and reduced patient stress or anxiety.
Does this mean that we are skeptical of extreme rehab – no, not at all! Interest, participation and development in fast track thoracic surgery programs continues to grow despite these obstacles.
In fact, the tightening of many federal and state restrictions on narcotics due to the American opioid crisis may make this the best time in modern American medical history to bring this ideas and approaches to our patients (Bruera & Del Fabbio, 2018, Herzid, 2018). It also means that many of us have some preliminary hurdles and preconceived notions (on all sides) to overcome to engage our patients, nurses, therapists and fellow medical professionals to get their buy-in on the idea. We might be over a decade behind – but it’s not too late to start today.
References:
Das-Neves-Pereira, et al. 2009). Fast track rehabilitation for lung cancer lobectomy: a five year experience. European Journal of Cardio-thoracic surgery, 36 (2009) 838-392. primary reference article.
Additional references:
Bruera, E. & Del Fabbio, E. (2018). Pain management in the era of the opioid crisis. Am Soc Clin Oncol Educ Book 2018 May 23 (38): 807-812.
D’Andrilli, A. & Rendina, E. (2018). Enhanced recovery after surgery and fast-track in video-assisted thoracic surgery lobectomy: preoperative optimisation and care-plans. Journal of visualized surgery, 2018:4 (4).
Herzid, S. (2018). Annals for hospitalists Inpatient Notes: Managing acute pain in the hospital in the face of the opioid crisis. Annals of internal medicine 169(6): H02-H03.
Rogers, et. al (2018). The impact of enhanced recovery after surgery (ERAS) protocol compliance on morbidity from resection for primary lung cancer. Journal of thoracic and cardiovascular surgery. 155(4) April 2018: 1843 -1852.
European Society of Anaesthesiology. “Hypnosis/local anesthesia combination during surgery helps patients, reduces hospital stays, study finds.” ScienceDaily. ScienceDaily, 21 June 2011.
From the Journal of thoracic disease – special issue: Supplemental issue #4 2018
Ardo et. al. (2018). Enhanced recovery pathways in thoracic surgery.
Bertani et al. (2018). A comprehensive protocol for physiokinesis therapy and enhanced recovery after surgery in patients undergoing video assisted thoracoscopic surgery: lobectomy.
Picconi, et. al. (2018). Enhanced recovery pathways in thoracic surgery from Italian VATS group: perioperative analgesic protocols.
Refai et. al. (2018). Enhanced recovery after thoracic surgery: patient information and care-plans.